Diabetes mellitus is often described as “starving in the land of plenty” meaning that every cell in the body, and in particular the central nervous system, needs sugar, the gasoline or fuel of the body, to function properly. However, in order for this “fuel” (sugar) to properly enter the body it requires a hormone called insulin that is produced by thousands of tiny little islands of cells (islets of langerhans) laced throughout the pancreatic organ.
The pancreas has two major and diverse functions:
The exocrine portion makes up the majority of the pancreas and produces the potent digestive enzymes that breaks down food into smaller particles for absorption and fuel; and the other major function, in lesser amounts, is the endocrine portion that synthesizes and releases several hormones into the bloodstream with insulin being the most important of these.
Pancreas
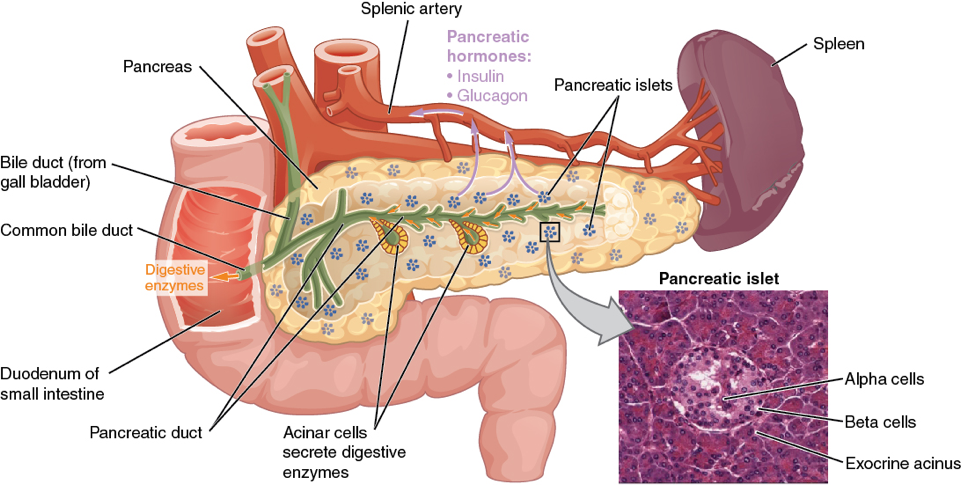
(Micrograph provided by the Regents of University of Michigan Medical School © 2012)
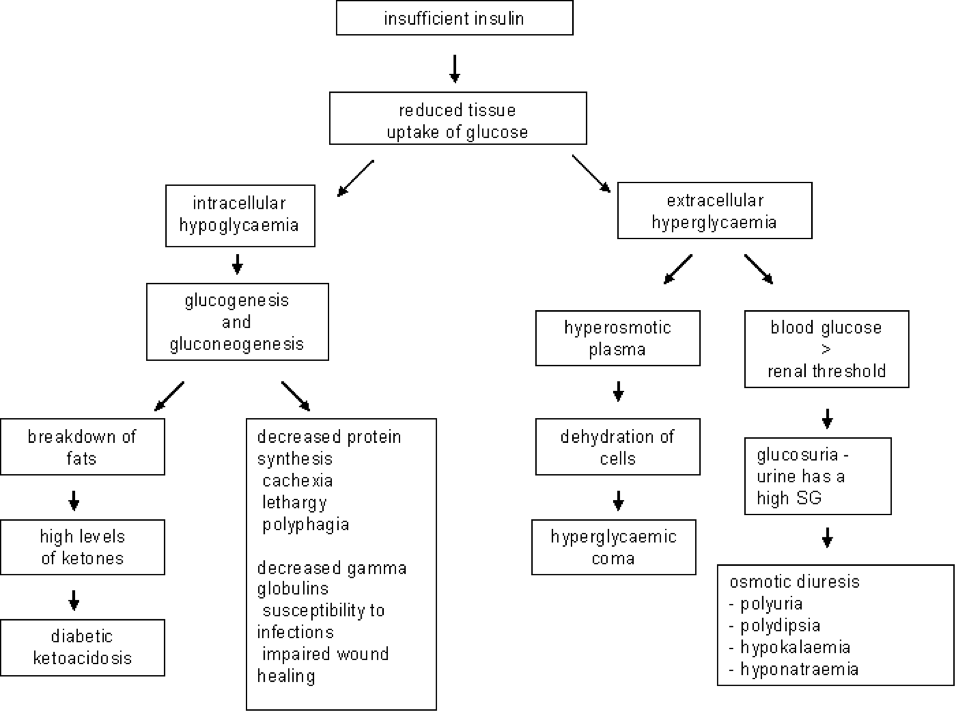
When the pancreas fails to produce enough insulin; the body is in a state of crying for help:
“give me energy, give me sugar, give me fuel to function”, but with suboptimal levels of insulin available the glucose (sugar) cannot effectively move from the bloodstream into the body cell.
In essence, the body is literally “starving to death in the land of plenty” meaning there is plenty of available glucose (fuel) in the bloodstream, but without insulin it’s just not getting to where it is needed the most; which is every cell in the body.
This leads to a number of negative metabolic abnormalities with the most common signs being an increase in thirst and urinations; panting; diminished to no appetite; vomiting, weight loss and generalized malaise. The “net effect”, when insulin is unavailable, is the body is in desperate need for fuel and starts to break down its own body fats as a poorer source of utilizable fuel. Eventually, this leads to an overwhelming increase in body acids (ketoacidosis) which leads to even more serious signs of dehydration, loss of appetite, malaise, vomiting, sepsis, coma and eventual death.
Pathophysiology of Diabetes Mellitus
The Main Clinical Signs of Diabetes Mellitus are:
- Increased thirst
- Increased urination
- Voracious appetite initially and diminished when the condition worsens
- Weight loss due to fat breakdown and loss of appetite
- Urinary tract infections are a common finding
- Cataracts
- Vomiting, panting, dull, coma, and death
Classification of Diabetes Mellitus
Diabetes mellitus is classified as either Type I or Type II as well as other subcategories.
Type I form of diabetes, also referred to as “insulin dependent diabetes”, is defined as an “absolute lack of” or “suboptimal amounts of” insulin production. Animals with Type I diabetes require insulin by injection for survival … for life.
This is by far the most common form of diabetes we see in the dog with the most common underlying cause being inflammation and destruction of the pancreatic islet cells due to pancreatitis; autoimmune disease; drugs; etc..
Type II form of diabetes, also referred as “non-insulin dependent diabetes” occurs due to one of several possibilities:
Obesity is by far the most common cause of Type II diabetes in humans and animals. Acromegaly (excessive growth hormone), Cushing’s syndrome (excessive cortisone) and various drugs are common contributing factors that lead to an increased demand by the body for higher than normal amounts of insulin (insulin resistance). This is the body’s attempt to maintain a normal blood sugar, in the face of these various insulin resistant factors, by producing higher amounts of insulin to overcome these resistances. With time, this constant demand for more insulin results in islet cell exhaustion, low insulin production, high blood sugar and full blown diabetes in both the dog and cat.
However, the most common finding, peculiar to cats with diabetes, is the finding of a non-dissolvable and non-treatable substance, called amyloid, that deposits within these insulin producing islet cells. This amyloid deposition results in a slow, but progressive, destruction of the insulin producing islet cells. The remaining viable islet cells still have the capability of producing insulin, but often in suboptimal amounts and not enough to keep up with the normal feline metabolic requirements. These cats will often require insulin management initially, but many can be weaned off insulin injections and regulated with dietary manipulations, weight reduction, and oral hypoglycemic drugs. However, the vast majority of these animals will eventually require insulin injections as their Type II diabetes, with further islet destruction by amyloid, progresses to Type I diabetes and they become insulin dependent.
Paul G. Cavanagh, DVM, DACVIM (SAIM)
Future Articles by Dr. Cavs:
Insulin & Oral Hypoglycemics; Diabetic Testing: what do they mean and why do we need them?; Diet in Diabetics: The Carnivore Connection;