
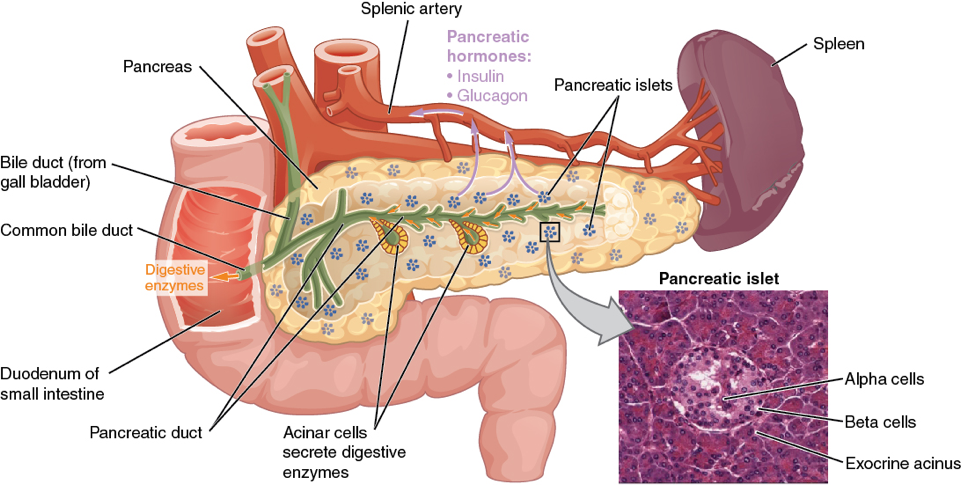
Diabetes mellitus is often described as “starving in the land of plenty” meaning that every cell in the body, and in particular the central nervous system, needs sugar, the gasoline or fuel of the body, to function properly. However, in order for this “fuel” (sugar) to properly enter the body it requires a hormone called insulin that is produced by thousands of tiny little islands of cells (islets of langerhans) laced throughout the pancreatic organ.
The pancreas has two major and diverse functions:
The exocrine portion makes up the majority of the pancreas and produces the potent digestive enzymes that breaks down food into smaller particles for absorption and fuel; and the other major function, in lesser amounts, is the endocrine portion that synthesizes and releases several hormones into the bloodstream with insulin being the most important of these.
Pancreas
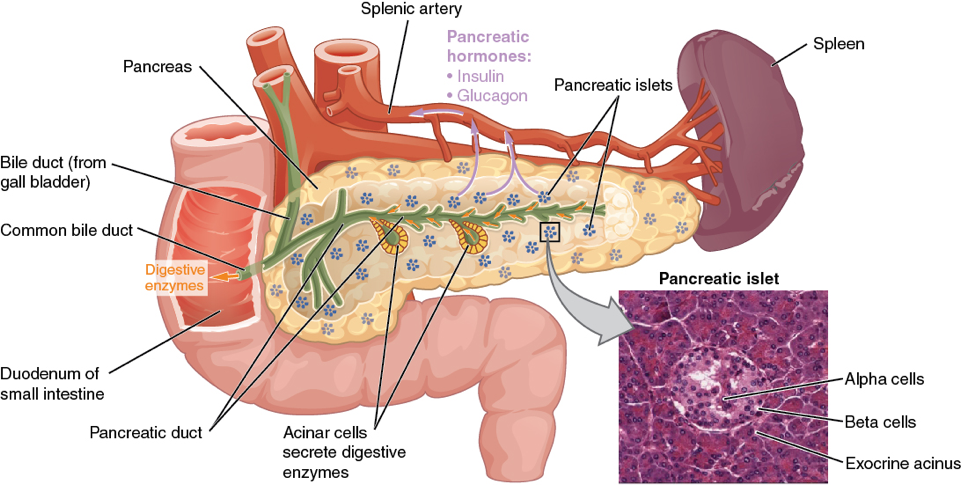
(Micrograph provided by the Regents of University of Michigan Medical School © 2012)
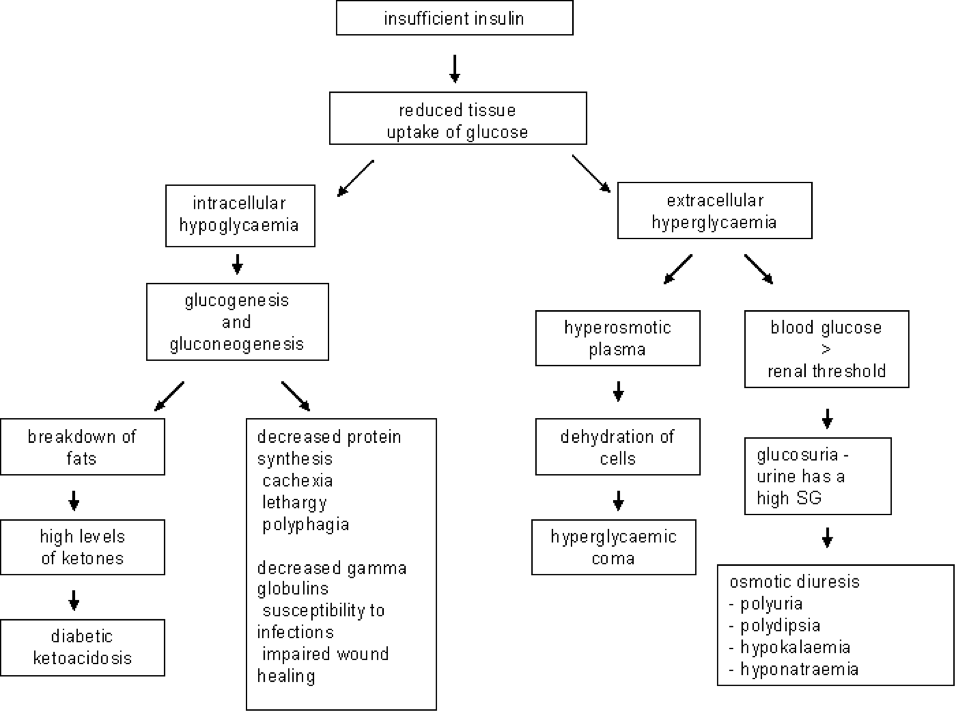
When the pancreas fails to produce enough insulin; the body is in a state of crying for help:
“give me energy, give me sugar, give me fuel to function”, but with suboptimal levels of insulin available the glucose (sugar) cannot effectively move from the bloodstream into the body cell.
In essence, the body is literally “starving to death in the land of plenty” meaning there is plenty of available glucose (fuel) in the bloodstream, but without insulin it’s just not getting to where it is needed the most; which is every cell in the body.
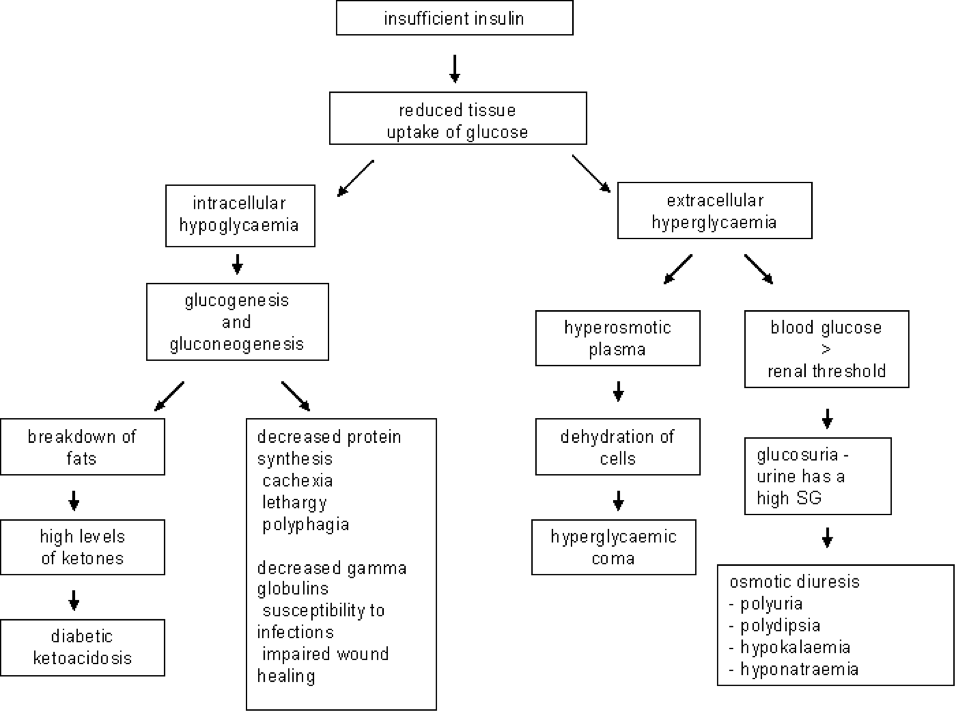
This leads to a number of negative metabolic abnormalities with the most common signs being an increase in thirst and urinations; panting; diminished to no appetite; vomiting, weight loss and generalized malaise. The “net effect”, when insulin is unavailable, is the body is in desperate need for fuel and starts to break down its own body fats as a poorer source of utilizable fuel. Eventually, this leads to an overwhelming increase in body acids (ketoacidosis) which leads to even more serious signs of dehydration, loss of appetite, malaise, vomiting, sepsis, coma and eventual death.
Pathophysiology of Diabetes Mellitus
The Main Clinical Signs of Diabetes Mellitus are:
- Increased thirst
- Increased urination
- Voracious appetite initially and diminished when the condition worsens
- Weight loss due to fat breakdown and loss of appetite
- Urinary tract infections are a common finding
- Cataracts
- Vomiting, panting, dull, coma, and death
Classification of Diabetes Mellitus
Diabetes mellitus is classified as either Type I or Type II as well as other subcategories.
Type I form of diabetes, also referred to as “insulin dependent diabetes”, is defined as an “absolute lack of” or “suboptimal amounts of” insulin production. Animals with Type I diabetes require insulin by injection for survival … for life.
This is by far the most common form of diabetes we see in the dog with the most common underlying cause being inflammation and destruction of the pancreatic islet cells due to pancreatitis; autoimmune disease; drugs; etc..
Type II form of diabetes, also referred as “non-insulin dependent diabetes” occurs due to one of several possibilities:
Obesity is by far the most common cause of Type II diabetes in humans and animals. Acromegaly (excessive growth hormone), Cushing’s syndrome (excessive cortisone) and various drugs are common contributing factors that lead to an increased demand by the body for higher than normal amounts of insulin (insulin resistance). This is the body’s attempt to maintain a normal blood sugar, in the face of these various insulin resistant factors, by producing higher amounts of insulin to overcome these resistances. With time, this constant demand for more insulin results in islet cell exhaustion, low insulin production, high blood sugar and full blown diabetes in both the dog and cat.
However, the most common finding, peculiar to cats with diabetes, is the finding of a non-dissolvable and non-treatable substance, called amyloid, that deposits within these insulin producing islet cells. This amyloid deposition results in a slow, but progressive, destruction of the insulin producing islet cells. The remaining viable islet cells still have the capability of producing insulin, but often in suboptimal amounts and not enough to keep up with the normal feline metabolic requirements. These cats will often require insulin management initially, but many can be weaned off insulin injections and regulated with dietary manipulations, weight reduction, and oral hypoglycemic drugs. However, the vast majority of these animals will eventually require insulin injections as their Type II diabetes, with further islet destruction by amyloid, progresses to Type I diabetes and they become insulin dependent.
Paul G. Cavanagh, DVM, DACVIM (SAIM)
Future Articles by Dr. Cavs:
Insulin & Oral Hypoglycemics; Diabetic Testing: what do they mean and why do we need them?; Diet in Diabetics: The Carnivore Connection;

Zika Virus and Animals
March 7, 2016 (published)
J.Scott Weese, DVM. DACVIM
I’ve been getting a lot of questions about Zika virus and animals. It’s great lo see that people are thinking more broadly about infectious diseases (but it isn’t doing much for my productivity this week).
To recap, Zika virus is a mosquito-borne virus related lo West Nile virus and dengue virus. Most people that are infected don’t get sick at all, and when they do, they usually get only mild signs of illness that resolve on their own. In the past few years, Zika virus has emerged in the Americas, particularly Brazil. Very recently, a link (still unproven) between infection of pregnant women and birth defects (babies born with small heads and brains [microcephaly]) has been reported, predominantly in Brazil.
Anti mosquito sign ,flat icon, vector
Can animals get infected with Zika virus?
- It depends on what you include in “animals.” We could be technical and say that humans are animals.
- Beyond that. non-human primates are susceptible. Zika was first identified in 1947 when
yellow fever researchers working in the Zika forest in Uganda stumbled onto it. They had a macaque in a cage and it developed a febrile illness from something that was transmissible. The virus was described as Zika virus in 1952 and then found in people a couple of years later.
But can domestic animals gel infected with Zika virus?
- Again, we need to think about the question. Infected means they get exposed lo the virus and it replicates in the body. That may occur, but we don’t have any evidence of it at this point.
- The more relevant question is whether animals can get sick from Zika virus exposure, and there’s also no evidence of that to date.
- A third aspect is whether infected (but potentially healthy) animals could be a reservoir for the virus, being able to pass it on to mosquitoes. There’s no evidence of that. either.
 So, the clearest answer is probably “maybe.” When it was a flu-like illness confined to some regions in Africa, Zika wasn’t a high priority so research hasn’t been extensive. The risk to pets in areas where the virus is circulating (areas where there are Aedes egpyti and Aedes albopictus mosquitoes) is probably very low. It would be good to look into the risks associated with domestic animals, including their susceptibility to disease and potential roles as reservoirs, but the likelihood that there is a relevant issue with either of these is probably remote.
So, the clearest answer is probably “maybe.” When it was a flu-like illness confined to some regions in Africa, Zika wasn’t a high priority so research hasn’t been extensive. The risk to pets in areas where the virus is circulating (areas where there are Aedes egpyti and Aedes albopictus mosquitoes) is probably very low. It would be good to look into the risks associated with domestic animals, including their susceptibility to disease and potential roles as reservoirs, but the likelihood that there is a relevant issue with either of these is probably remote.

Protecting your cat or dog (or both) from ticks is an important part of disease prevention. In fact, there are several diseases that can be transmitted to your pet from a tick bite. The four most common tick-borne diseases seen in the United States are Lyme disease, Anaplasma, Ehrlichia and Rocky Mountain Spotted Fever. Here we will briefly discuss these tick-borne diseases that affect both dogs and cats.



Lyme Disease
Also called borreliosis, Lyme disease is caused by the bacteria Borrelia burgdorferi. Deer ticks carry these bacteria, transmitting them to the animal while sucking its blood. The tick must be attached to the dog (or cat) for about 48 hours in order to transmit the bacteria to the animal’s bloodstream. If the tick is removed before this, transmission will usually not occur.
Common signs of Lyme disease include lameness, fever, swollen lymph nodes and joints, and a reduced appetite. In severe cases, animals may develop kidney disease, heart conditions, or nervous system disorders. Animals do not develop the tell-tale “lyme disease rash” that is commonly seen in humans with Lyme disease.
Blood tests are necessary to diagnose Lyme disease in pets. If the results are positive, oral antibiotics are given as treatment for the condition. Dogs that have already had Lyme disease are able to get the disease again — they are not immunized against it — so prevention is key. A vaccine for Lyme disease is available for dogs, but unfortunately, the vaccine is not available for cats. If you live in an area where these ticks are endemic, you should have your dogs vaccinated yearly.
Anaplasmosis
Deer ticks and western black-legged ticks carry the bacteria that transmit canine anaplasmosis. Another form of anaplasmosis (caused by a different bacteria) is carried by the brown dog tick. Both dogs and cats are at risk for this condition. Because the deer tick also carries other diseases, some animals may be at risk for developing more than one tick-borne disease at a time.
Signs of anaplasmosis are similar to ehrlichiosis and include pain in the joints, fever, vomiting, diarrhea, and possible nervous system disorders. Pets will usually begin to show signs of disease within a couple weeks after infection. Diagnosis of anaplasmosis will usually require blood tests, urine tests, and sometimes other specialized lab tests.
Oral antibiotics are given for up to a month for treatment of anaplasmosis, depending on the severity of the infection. When treated promptly, most pets will recover completely. Immunity is not guaranteed after a bout of anaplasmosis, so pets may be reinfected if exposed again.
Ehrlichiosis
Another tick-borne disease that affects dogs is ehrlichiosis. It is transmitted by the brown dog tick and the Lone Star Tick. This disease is caused by a rickettsial organism and has been seen in every state in the U.S., as well as worldwide. Common symptoms include depression, reduced appetite (anorexia), fever, stiff and painful joints, and bruising. Signs typically appear less than a month after a tick bite and last for about four weeks.
Special blood tests may be needed to test for antibodies to Ehrlichia. Antibiotics are usually given for up to four weeks to completely clear the organism. After infection, the animal may develop antibodies to the organism, but will not be immune to reinfection. There is no vaccine available for ehrlichiosis. Low doses of antibiotics may be recommended for animals during tick season in areas of the country that are endemic to this disease.

Tick prevention for Dogs breed Griffon Bruxellois
Rocky Mountain Spotted Fever
A disease seen commonly in dogs in the east, Midwest, and plains region of the U.S. is Rocky Mountain spotted fever (RMSF). Cats can be infected with RMSF, but the incidence is much lower for them. The organisms that cause RMSF are transmitted by the American dog tick and the Rocky Mountain spotted fever tick.
The tick must be attached to the dog or cat for at least five hours in order for transmission of the organism to occur. Signs of RMSF may include fever, reduced appetite, depression, pain in the joints, lameness, vomiting, and diarrhea. Some animals may develop heart abnormalities, pneumonia, kidney failure, liver damage, or even neurological signs (e.g., seizures, stumbling).
Blood tests can show antibodies to the organism, signifying that the animal has been infected. Oral antibiotics are used for about two weeks to treat the infection. Animals that are able to clear the organism will recover and remain immune to future infection. However, if your dog or cat has heart, liver, or kidney damage, and/or the nervous system has been affected by the infection, it may require additional supportive treatment, generally in hospital.
Currently, there is no vaccine available to prevent RMSF, so tick control is very important for animals living in endemic areas.
By Jennifer Kvamme, DVM from mypetMD
Edited by Paul G. Cavanagh, DVM, DACVIM (SAIM)


 So, the clearest answer is probably “maybe.” When it was a flu-like illness confined to some regions in Africa, Zika wasn’t a high priority so research hasn’t been extensive. The risk to pets in areas where the virus is circulating (areas where there are Aedes egpyti and Aedes albopictus mosquitoes) is probably very low. It would be good to look into the risks associated with domestic animals, including their susceptibility to disease and potential roles as reservoirs, but the likelihood that there is a relevant issue with either of these is probably remote.
So, the clearest answer is probably “maybe.” When it was a flu-like illness confined to some regions in Africa, Zika wasn’t a high priority so research hasn’t been extensive. The risk to pets in areas where the virus is circulating (areas where there are Aedes egpyti and Aedes albopictus mosquitoes) is probably very low. It would be good to look into the risks associated with domestic animals, including their susceptibility to disease and potential roles as reservoirs, but the likelihood that there is a relevant issue with either of these is probably remote.



